Free Do Not Resuscitate Order Form for Texas
When it comes to making decisions about end-of-life care, understanding the options available is crucial for individuals and their families. In Texas, one important tool at the disposal of those facing such critical decisions is the Do Not Resuscitate (DNR) Order form. This form plays a pivotal role in directing healthcare professionals not to perform cardiopulmonary resuscitation (CPR) if a person's breathing stops or if the heart stops beating. It's a deeply personal decision, often made after thoughtful conversation with loved ones and healthcare providers, to ensure that a person's wishes are respected in their final moments. The Texas DNR Order form requires careful consideration of its implications, legal requirements, and the process for its completion and execution. Understanding all these aspects ensures that individuals can make informed choices about their end-of-life care preferences, aligning medical interventions with their values and desires.
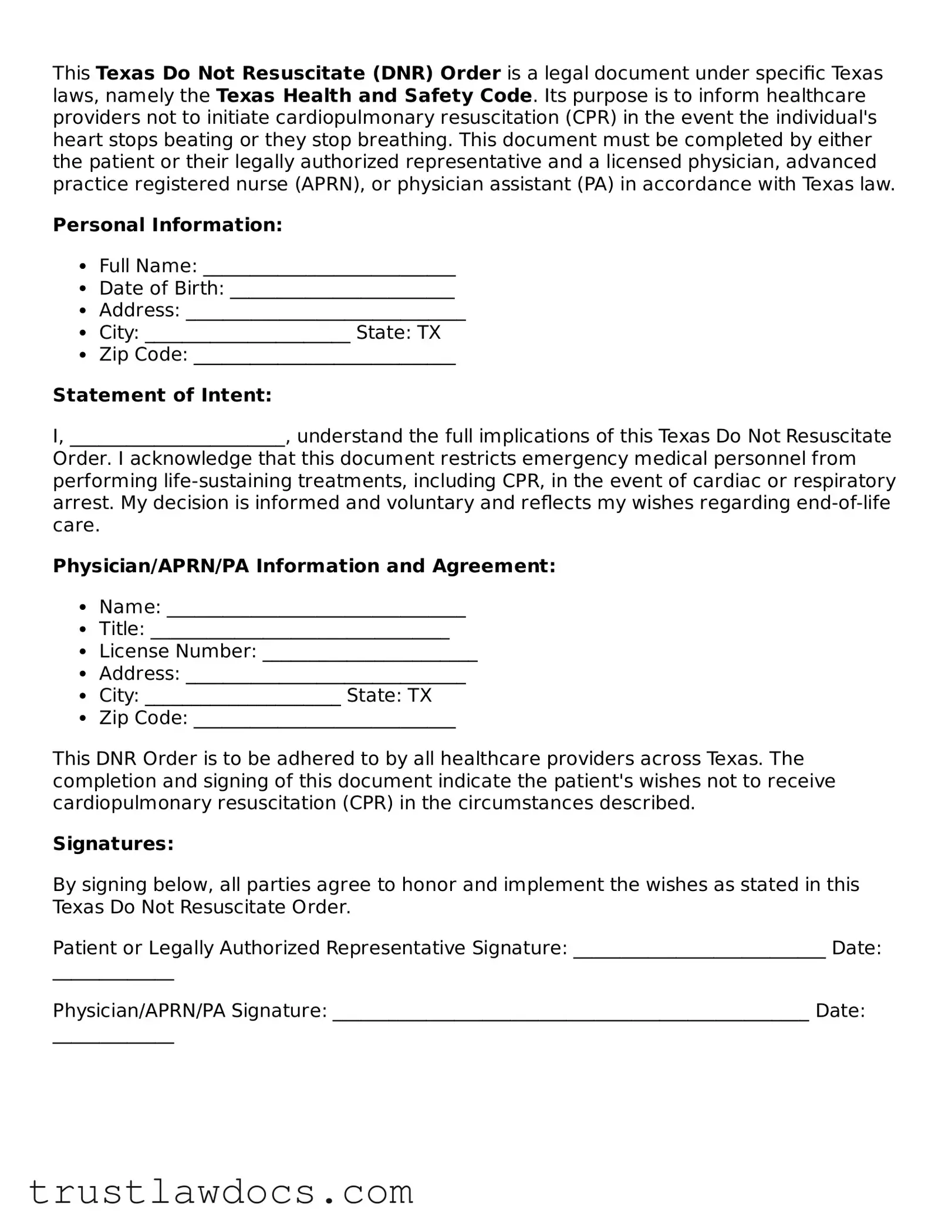
Form Example
This Texas Do Not Resuscitate (DNR) Order is a legal document under specific Texas laws, namely the Texas Health and Safety Code. Its purpose is to inform healthcare providers not to initiate cardiopulmonary resuscitation (CPR) in the event the individual's heart stops beating or they stop breathing. This document must be completed by either the patient or their legally authorized representative and a licensed physician, advanced practice registered nurse (APRN), or physician assistant (PA) in accordance with Texas law.
Personal Information:
- Full Name: ___________________________
- Date of Birth: ________________________
- Address: ______________________________
- City: ______________________ State: TX
- Zip Code: ____________________________
Statement of Intent:
I, _______________________, understand the full implications of this Texas Do Not Resuscitate Order. I acknowledge that this document restricts emergency medical personnel from performing life-sustaining treatments, including CPR, in the event of cardiac or respiratory arrest. My decision is informed and voluntary and reflects my wishes regarding end-of-life care.
Physician/APRN/PA Information and Agreement:
- Name: ________________________________
- Title: ________________________________
- License Number: _______________________
- Address: ______________________________
- City: _____________________ State: TX
- Zip Code: ____________________________
This DNR Order is to be adhered to by all healthcare providers across Texas. The completion and signing of this document indicate the patient's wishes not to receive cardiopulmonary resuscitation (CPR) in the circumstances described.
Signatures:
By signing below, all parties agree to honor and implement the wishes as stated in this Texas Do Not Resuscitate Order.
Patient or Legally Authorized Representative Signature: ___________________________ Date: _____________
Physician/APRN/PA Signature: ___________________________________________________ Date: _____________
PDF Form Details
| Fact Name | Description |
|---|---|
| Definition | A Texas Do Not Resuscitate (DNR) Order form is a legal document indicating that a person does not want to receive cardiopulmonary resuscitation (CPR) if their heart stops or if they stop breathing. |
| Applicability | This form is valid only within the state of Texas. |
| Governing Law | The Texas Health and Safety Code, specifically sections 166.081 through 166.091, governs the issuance of Do Not Resuscitate Orders. |
| Who Can Issue | The form must be signed by a physician to be considered valid and can be based on an individual’s or their legally authorized representative’s directions. |
| Effective Location | It is effective in various settings within Texas, including hospitals, in-patient settings, and at the patient's home. |
| Form Requirements | The form requires the patient's or the legally authorized representative’s signature, the physician's signature, and the date to be considered valid. |
| Revocation | The DNR order can be revoked by the patient or their legally authorized representative at any time, through written or oral communication to the physician or healthcare provider. |
| Recognition | Emergency medical services (EMS) personnel are required to honor a valid Texas DNR order presented to them during emergency situations. |
How to Write Texas Do Not Resuscitate Order
Deciding not to undergo cardiopulmonary resuscitation (CPR) in the event of a cardiac or respiratory arrest is a significant choice. In Texas, formalizing this decision requires completing a Do Not Resuscitate (DNR) Order form. This document ensures that healthcare providers and emergency medical services respect your wishes. Filling out the form correctly is crucial for it to be valid, so following each step carefully is important.
Here are the steps needed to accurately complete the Texas Do Not Resuscitate Order form:
- Start by providing the patient's full legal name to ensure the DNR Order is correctly identified with the individual it pertains to.
- Next, include the patient’s date of birth, which is essential for further verification of identity.
- Enter the patient's address, including city, state, and zip code, to provide a complete identification context.
- If applicable, specify the patient's Texas Driver's License or ID number. This is an optional step but can add another layer of identification.
- Include a brief description of the patient’s medical condition. This helps clarify the context in which the DNR Order is being requested.
- The form must be signed and dated by the patient, or if the patient is unable, a legally authorized person can do so on their behalf. This signature is a critical element, making the document legally binding.
- A physician's signature is also required for the form to be valid. The doctor will review the patient's condition and the decision for a DNR Order, providing their professional validation of the request.
- Finally, keep the completed and signed form in a place where it can be easily accessed by healthcare providers or family members, such as with other important medical documents or shared with a primary care provider.
Once the Texas Do Not Resuscitate Order form is filled out and properly signed, it represents your clear directive regarding CPR in emergencies. It’s a personal decision that legally ensures your healthcare preferences are respected, giving you and your loved ones peace of mind. Remember to discuss this decision with your healthcare provider and loved ones to ensure everyone is informed.
Get Answers on Texas Do Not Resuscitate Order
What is a Texas Do Not Resuscitate (DNR) Order form?
A Texas DNR Order form is a document used by a patient or their legal representative to inform medical professionals that they do not want to receive cardiopulmonary resuscitation (CPR) in the event their breathing stops or their heart stops beating. This order is used to ensure the patient's wishes are respected during emergency situations or at the end of life.
Who can fill out a Texas DNR Order form?
The form can be filled out by an adult patient who is competent to make their own medical decisions, a legally authorized representative if the patient is unable to make their own decisions, or by the parent or guardian of a minor child. Competency and the ability to make informed decisions are key factors in this process.
Where does a Texas DNR Order need to be placed?
Once completed and signed by the appropriate parties, the DNR Order should be placed in a location where it can be easily found by emergency responders or medical personnel. This might include placing it on the refrigerator, in a personal health record, or with other important medical documents. Some individuals may also choose to wear a DNR bracelet to indicate their wishes.
Is the Texas DNR Order form recognized across state lines?
While a Texas DNR Order is legally binding within the state of Texas, its recognition may vary in other states. Each state has its own laws and regulations regarding DNR orders. If you travel or move to another state, it's important to review that state's requirements and possibly complete a new form according to their laws.
How can a Texas DNR Order be revoked?
A Texas DNR Order can be revoked at any time by the person who created it. This can be done through a verbal statement to a healthcare provider or by physically destroying the DNR Order form and any DNR identification bracelets or documents. It is crucial that all healthcare providers are informed of the revocation to ensure the patient's current wishes are honored.
Does having a Texas DNR Order affect the quality of care received?
No, having a DNR Order does not affect the quality of care one receives. Healthcare professionals are committed to providing the best possible care to all patients. The DNR Order specifically addresses the use of CPR in emergency situations where the heart or breathing has stopped and does not impact other treatments or care provided.
Can a Texas DNR Order be modified?
Yes, a DNR Order can be modified if the patient's wishes change. To modify a DNR Order, a new form should be completed and signed, reflecting the current decisions of the patient or their legal representative. It is important to communicate any changes to the DNR Order to all involved in the patient's care, including family members and healthcare providers.
Common mistakes
Filling out a Do Not Resuscitate (DNR) order in Texas requires careful attention to detail and a deep understanding of the wishes of the person it pertains to. Unfortunately, mistakes are common, leading to potentially unwanted interventions or, conversely, a lack of critical care. One prevalent error is incomplete information. Every field on the Texas DNR form should be carefully filled out to prevent any ambiguity about the patient’s wishes.
Another frequent oversight is not securing the necessary signatures. For a Texas DNR to be valid, it must be signed by the individual (or their legally authorized representative) and the physician. Missing signatures can render the document ineffective, causing unnecessary stress or legal battles during emergencies. Similarly, failing to date the form can also create confusion regarding its validity, especially if the person's health status or wishes have changed since it was filled out.
A common confusion arises when people mistake a Texas DNR with an advance directive. While both documents relate to end-of-life wishes, they serve different purposes. A DNR specifically addresses the desire not to have CPR in the event of a cardiac or respiratory arrest, whereas an advance directive may cover a broader spectrum of decisions, such as artificial nutrition or mechanical ventilation preferences. Mixing up these documents or assuming one substitutes for the other is a critical mistake.
Additionally, not informing family members or caregivers about the existence and content of the DNR order is a significant oversight. In the chaos of an emergency, healthcare providers may turn to family or close associates for guidance. If these individuals are unaware of the DNR, they might unknowingly contradict its instructions. Moreover, failure to keep the DNR accessible can also thwart its intent. Hospital personnel and emergency responders need to easily find the document during crises.
There’s also a tendency to overlook state-specific requirements. Texas, like every state, has its own laws regarding DNR orders. Assuming that DNR directives from another state automatically apply in Texas could lead to a crucial misunderstanding of the patient's end-of-life wishes not being honored as intended. Furthermore, not updating the DNR after significant health changes is another common error. As health conditions evolve, so too might decisions regarding emergency medical interventions.
Ignoring legal representation consultation is another pitfall. Legal advice can help ensure that a DNR aligns with other estate planning documents and Texas laws, preventing legal complications down the line. Lastly, a mistake often made is not reviewing and reaffirming the document periodically. Regular reviews help confirm that the DNR reflects the current wishes of the individual, taking any new medical diagnoses or life changes into account.
Avoiding these mistakes when completing a Texas DNR requires diligence, open communication with healthcare professionals, and thoughtful consideration of the person's end-of-life wishes. It’s a significant step in honoring the autonomy and values of individuals as they navigate their healthcare journeys.
Documents used along the form
Completing a Texas Do Not Resuscitate (DNR) Order form is a significant step in planning for medical care, especially when it comes to decisions about end-of-life treatment. However, this form is often part of a larger set of legal and medical documents designed to ensure a person's healthcare wishes are followed. Understanding these documents can provide a comprehensive approach to healthcare planning.
- Medical Power of Attorney (POA) – This document allows an individual to appoint someone else to make medical decisions on their behalf if they become unable to do so. It's crucial for situations where medical decisions need to be made, and the individual cannot communicate their wishes.
- Living Will – A living will is a written document that specifies what types of medical treatment are desired or not desired by an individual at the end of their life. This can include treatments that prolong life, such as artificial respiration or tube feeding.
- Physician Orders for Scope of Treatment (POST) – This form provides specific instructions about a patient’s healthcare preferences, including resuscitation. It is used primarily by individuals with serious illnesses or at the end of life.
- Out-of-Hospital Do Not Resuscitate (OOH-DNR) order – Similar to the DNR, this document specifically directs emergency medical personnel not to perform CPR or other life-sustaining treatments in non-hospital settings.
- Advance Healthcare Directive – This is a broader document that can include a living will, DNR orders, and medical POA, specifying a wide range of preferences about end-of-life care and treatments.
- HIPAA Release Form – The Health Insurance Portability and Accountability Act (HIPAA) release form allows healthcare providers to share your health information with designated individuals, often those also named in a medical POA or living will.
- Declaration for Mental Health Treatment – This document specifies what mental health treatments an individual wants or does not want if they are diagnosed with a mental disorder and are incapable of making decisions.
Together, these documents form a comprehensive plan that respects the healthcare wishes of an individual when they cannot speak for themselves. Each serves its unique purpose, from specifying medical treatments to appointing decision-makers, and ensures that healthcare providers and loved ones understand and respect those wishes. It's advisable for individuals to consult with legal and healthcare professionals to ensure these documents are correctly completed and filed.
Similar forms
The Living Will is quite similar to the Texas Do Not Resuscitate (DNR) Order as both documents guide healthcare providers about a patient's preferences in life-sustaining treatments. Living Wills typically cover a broader range of medical interventions and end-of-life care decisions, whereas DNR Orders specifically address the use of CPR (cardiopulmonary resuscitation) in the event of a cardiac or respiratory arrest.
Medical Power of Attorney forms also share similarities with DNR Orders, as both involve directives for healthcare. While a DNR Order explicitly refuses certain life-saving treatments, a Medical Power of Attorney designates an individual to make healthcare decisions on behalf of someone who is unable to do so, potentially covering a wide range of medical decisions beyond resuscitation instructions.
The Advance Directive is another document related to a DNR Order, combining elements of both a Living Will and a Medical Power of Attorney. It outlines a person's healthcare preferences, including intervention wishes and nomination of a decision-maker, if the individual can't communicate those decisions due to a medical condition, thereby encompassing the intent behind a DNR.
A POLST (Physician Orders for Life-Sustaining Treatment) form is closely related to a DNR Order as it offers medical orders about certain life-sustaining treatments based on a patient's current health condition. Unlike a DNR that primarily focuses on CPR, a POLST can provide broader instructions concerning intubation, mechanical ventilation, and other interventions.
HIPAA Release Forms, while primarily focused on the privacy and sharing of an individual's health information, intersect with DNR Orders in the context of healthcare decision-making. They ensure that healthcare providers can share vital health information with designated individuals, who might need access to this information to make informed decisions about DNR directives and other healthcare matters.
A Hospital Admission Form, often filled out upon entering a hospital, can include information relevant to a patient's DNR status. These forms capture a wide array of health-related information, including existing DNR Orders, to inform the hospital staff of the patient's wishes and medical directives upon admission.
An Emergency Medical Services (EMS) Protocol could be akin to a DNR Order in emergency medical situations. EMS protocols guide first responders and paramedics in treating patients in the field, where an existing DNR Order would dictate specific actions, such as not performing CPR on a patient who has elected for this in their healthcare directives.
A Healthcare Proxy form nominates a person to make healthcare decisions on someone's behalf, similar to a Medical Power of Attorney. Although it doesn't address specific treatments like a DNR Order, it's another tool for ensuring that a patient's healthcare wishes are respected, especially when they cannot speak for themselves.
A Five Wishes Document goes beyond traditional medical directives by addressing personal, emotional, and spiritual needs alongside medical wishes, like a DNR. It includes who the individual wants to make decisions for them, the kind of medical treatment they want or don't want, how comfortable they wish to be, how they want to be treated, and what they want their loved ones to know.
Last Will and Testament forms, primarily used for after-death affairs, indirectly relate to DNR Orders by reflecting an individual's wishes regarding their properties and dependents. While distinctly different in application—DNR Orders address immediate medical intervention preferences—they are similar in spirit, with both documents outlining directives to be followed upon the individual's incapacity or death.
Dos and Don'ts
When filling out the Texas Do Not Resuscitate (DNR) Order form, it's important to ensure accuracy and completeness to respect the wishes of the individual for whom the form is being completed. Here is a list of things you should and shouldn't do:
Do:- Verify the patient's identity to ensure the DNR order is attributed correctly.
- Consult with a healthcare professional if you are uncertain about any medical terms or implications.
- Ensure the form is filled out completely, leaving no required fields blank.
- Include the date when the DNR order was signed to confirm its validity.
- Ensure both the patient (or legally authorized representative) and the physician sign the form to make it legally binding.
- Don't fill out the form without the consent of the patient or their legally authorized representative.
- Don't use unclear or vague language; be precise in your wording to avoid any misunderstandings.
- Don't forget to review the form for any errors before submitting it.
- Don't lose or misplace the form; keep it in a safe and accessible place for healthcare providers.
Misconceptions
When it comes to understanding the Texas Do Not Resuscitate (DNR) Order form, several misconceptions can cloud one's judgment. It is essential to clear up these misunderstandings to make informed decisions about health care and emergency medical services. Below are ten common misconceptions about the Texas DNR Order form:
Anyone can create a DNR Order for themselves at any time. False. Only adults with the capacity to make their own medical decisions or their legally authorized representatives can issue a Texas DNR Order.
A DNR Order is only for the elderly. Incorrect. A DNR Order can apply to any patient, regardless of age, who wishes to refuse CPR or advanced cardiac life support techniques in the event of cardiac or respiratory arrest, based on their health condition and personal wishes.
DNR Orders apply in all medical situations. Not true. A DNR Order specifically addresses the refusal of CPR techniques in the event of cardiac or respiratory arrest and does not apply to other medical interventions or treatments.
Having a DNR means you will not receive any medical treatment. Misconception. A DNR Order only relates to the non-administration of CPR, not the refusal of other medical treatments or interventions that might be beneficial.
DNR Orders are permanent and cannot be changed. Incorrect. Patients or their legal representatives can revoke or modify a DNR Order at any time to reflect their current wishes.
A DNR Order must be on a specific form to be valid. False. While Texas has a standardized form, the most crucial factor is that the DNR Order complies with state laws and is clearly communicated to and understood by healthcare providers.
Hospital DNR Orders are effective outside the hospital. Not accurate. Hospital-issued DNR Orders may not apply in non-hospital settings. It's important to have a Texas Out-of-Hospital DNR Order for it to be recognized by emergency medical services outside hospital premises.
You need an attorney to complete a DNR Order. Not necessary. While legal advice can be helpful, particularly for complex cases, one does not need an attorney to complete a DNR Order in Texas.
DNR Orders mean "do not treat." A common misconception. A DNR Order only directs healthcare providers not to initiate CPR or advanced cardiac life support if a patient's heart stops or they stop breathing. It does not mean the patient will be denied other forms of care.
Only a doctor can issue a DNR Order. Misunderstanding. While a physician does need to sign the DNR Order for it to be valid, the initial request can come from the patient or their legally authorized representative.
It is critical to thoroughly discuss and understand all aspects of the Texas Do Not Resuscitate Order form with healthcare providers to ensure wishes are honored while respecting legal guidelines. Clearing up these misconceptions can lead to better informed decisions and peace of mind for patients and their families.
Key takeaways
The Texas Do Not Resuscitate (DNR) Order form is a critical document for individuals who wish to refuse certain life-sustaining treatments in the event of a cardiac or respiratory arrest. Understanding the nuances of this form is essential for making informed healthcare decisions and ensuring that one's end-of-life care preferences are respected. Here are key takeaways about filling out and using the Texas DNR Order form:
- Eligibility and Voluntary Execution: To fill out a Texas DNR Order, the individual must be of sound mind and capable of making healthcare decisions or legally authorized to do so on behalf of the patient. The decision to have a DNR Order is entirely voluntary and should be made after careful consideration and discussion with healthcare providers and loved ones.
- Need for Physician's Signature: A valid DNR Order in Texas requires the signature of a licensed physician. The physician's signature indicates that they have discussed the implications of a DNR Order with the patient (or their legal representative) and that they concur with the patient's decision to forego resuscitation efforts.
- Specific Interventions Refused: It's important to understand that a DNR Order specifically addresses the refusal of interventions meant to restart heart and lung function. These interventions include CPR (cardiopulmonary resuscitation), advanced airway management, and artificial ventilation. However, it does not preclude the patient from receiving other forms of medical treatment aimed at providing comfort or treating other medical conditions.
- Portability and Recognition: The Texas DNR Order is recognized statewide and should be kept in a place where it can be easily found by emergency personnel, such as with the patient or in a visible location within the home. When outside the home, individuals are advised to carry a wallet card indicating they have a DNR Order.
- Revocation Process: It is equally important to understand that the decision to have a DNR Order is reversible. Should the individual or their legal representative change their mind, the DNR Order can be revoked orally or in writing at any time, irrespective of the individual's mental or physical condition.
Ultimately, the Texas DNR Order form embodies the individual's right to make decisions regarding their end-of-life care. It ensures that these decisions are respected by health care professionals and protect individuals from receiving treatment they have expressly declined. As with any healthcare decision, it is advisable to consult with healthcare professionals and legal counsel to fully understand the implications and process of executing a DNR Order.
Popular Do Not Resuscitate Order State Forms
Florida Do Not Resuscitate Form - Legally supports a patient's right to decline specific medical treatments in circumstances of critical health decline.
Do Not Resuscitate Guidelines - The document is part of advance healthcare directives, aiming to empower individuals in their medical care decisions.
Where to Get Dnr Forms - Guidance for healthcare workers on a patient's clear decision to decline resuscitation attempts.
Dnr/dni Form - Facilitates clear communication between patients, their families, and healthcare providers regarding end-of-life care wishes.