Official Do Not Resuscitate Order Document
At the crossroads of personal healthcare decisions, the Do Not Resuscitate (DNR) Order form plays a quintessential role for individuals facing serious illness or at the end of their lives. This critical document, while simple in its concept, carries profound implications for patients, their families, and healthcare providers. It essentially instructs medical professionals not to perform CPR (cardiopulmonary resuscitation) or advanced cardiac life support if a patient's breathing stops or if the heart ceases beating. The choice to have a DNR in place is deeply personal and can be influenced by a myriad of factors including the patient's values, quality of life considerations, and medical advice. Understanding how to properly complete and maintain a DNR order, its legal status, and how it differs from other medical directives is crucial. This ensures that a patient's wishes are honored, and loved ones and medical teams are clear on those wishes. Delving into the specifics, nuances, and impacts of a DNR order form can empower individuals and families to make informed decisions about end-of-life care.
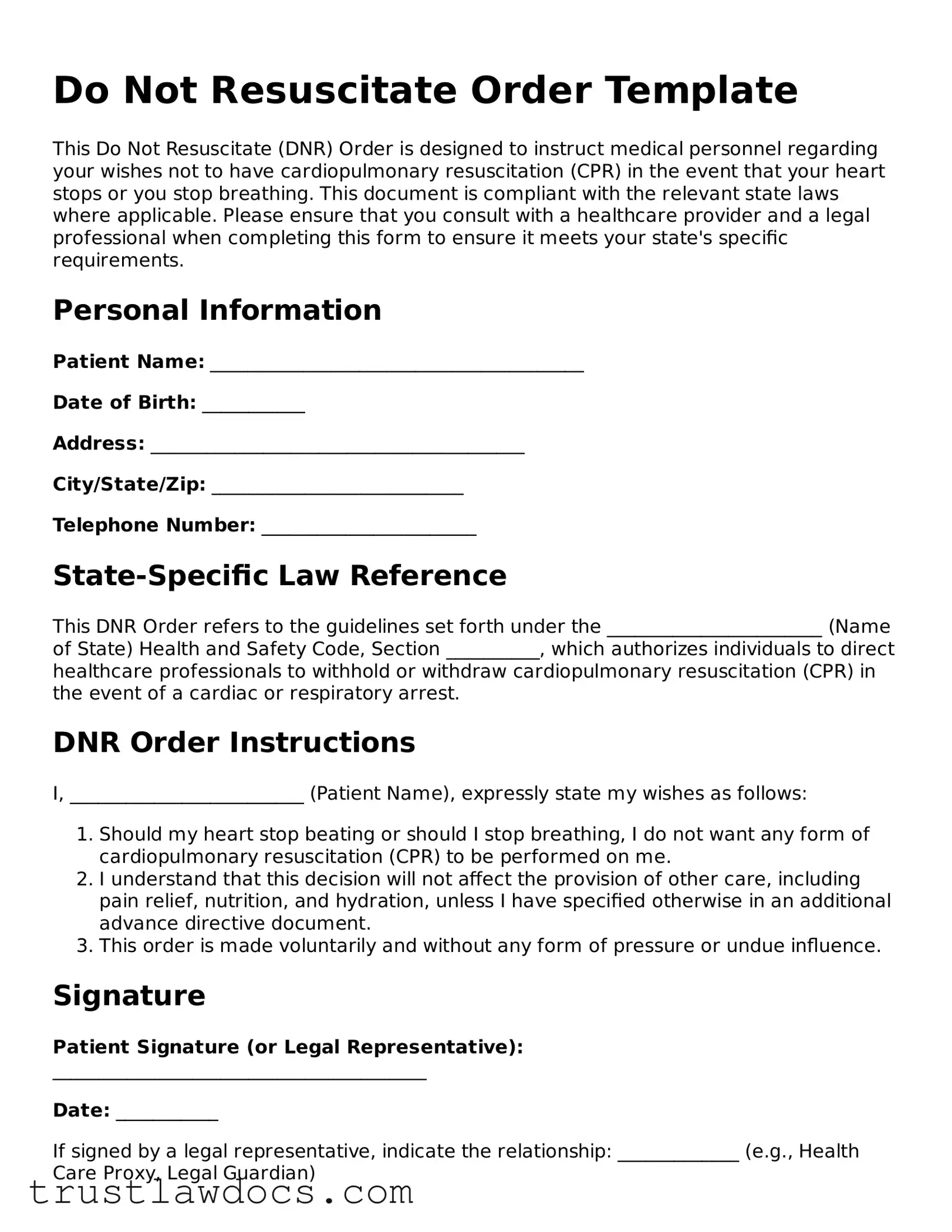
Form Example
Do Not Resuscitate Order Template
This Do Not Resuscitate (DNR) Order is designed to instruct medical personnel regarding your wishes not to have cardiopulmonary resuscitation (CPR) in the event that your heart stops or you stop breathing. This document is compliant with the relevant state laws where applicable. Please ensure that you consult with a healthcare provider and a legal professional when completing this form to ensure it meets your state's specific requirements.
Personal Information
Patient Name: ________________________________________
Date of Birth: ___________
Address: ________________________________________
City/State/Zip: ___________________________
Telephone Number: _______________________
State-Specific Law Reference
This DNR Order refers to the guidelines set forth under the _______________________ (Name of State) Health and Safety Code, Section __________, which authorizes individuals to direct healthcare professionals to withhold or withdraw cardiopulmonary resuscitation (CPR) in the event of a cardiac or respiratory arrest.
DNR Order Instructions
I, _________________________ (Patient Name), expressly state my wishes as follows:
- Should my heart stop beating or should I stop breathing, I do not want any form of cardiopulmonary resuscitation (CPR) to be performed on me.
- I understand that this decision will not affect the provision of other care, including pain relief, nutrition, and hydration, unless I have specified otherwise in an additional advance directive document.
- This order is made voluntarily and without any form of pressure or undue influence.
Signature
Patient Signature (or Legal Representative): ________________________________________
Date: ___________
If signed by a legal representative, indicate the relationship: _____________ (e.g., Health Care Proxy, Legal Guardian)
Physician Information and Endorsement
Physician Name: ________________________________________
License Number: _______________________
Address: ________________________________________
Telephone Number: _______________________
The undersigned physician affirms that the above-named patient has discussed the implications of this Do Not Resuscitate Order, is aware of their condition, and has made this request freely and without coercion.
Physician Signature: ________________________________________
Date: ___________
PDF Form Details
| Fact Number | Fact |
|---|---|
| 1 | A Do Not Resuscitate (DNR) Order form is a legal document that tells health care providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. |
| 2 | DNR orders are used when a person has a serious illness or is at the end of their life and wishes to die naturally without aggressive interventions. |
| 3 | The process for creating a DNR order varies by state, and it must comply with specific state laws regarding end-of-life decisions. |
| 4 | In many states, DNR orders must be signed by both the patient (or their legal healthcare power of attorney) and the patient's doctor. |
| 5 | DNR orders can be part of a larger advance healthcare directive or living will, documents that express a person’s wishes about medical treatment if they become unable to communicate. |
| 6 | Some states have specific forms, like the POLST (Physician Orders for Life-Sustaining Treatment), which include DNR orders along with other wishes regarding end-of-life care treatments. |
| 7 | It's important to have conversations with family and healthcare providers about one's end-of-life care preferences to ensure that a DNR order and other advance directives reflect those wishes. |
How to Write Do Not Resuscitate Order
Preparing a Do Not Resuscitate (DNR) Order is a significant step for anyone desiring specific end-of-life care measures. This document ensures that in the event of a cardiac or respiratory arrest, medical personnel will not perform CPR (cardiopulmonary resuscitation). Understanding and completing this document requires attention to detail and clarity on your part to ensure that your wishes are respected. Here's a straightforward guide to filling out your DNR Order form properly.
- Begin by gathering all necessary personal information, including your full legal name, date of birth, and address. This information helps identify you clearly and prevents any confusion.
- Read the entire form carefully before filling it out. This ensures you understand the implications of the document and the specifics of what you are agreeing to.
- In the section provided, enter your personal information accurately. Double-check spelling and details to avoid errors.
- Many DNR forms require specifying the conditions under which the DNR order should apply. If your form includes this section, clearly outline your wishes.
- Look for the section designated for your signature. Signing the form is crucial as it indicates your agreement and understanding of the DNR's purpose and conditions. Ensure you sign in the presence of a witness if required.
- If the form requests a witness signature, have an adult witness sign the form. Their signature verifies that you signed the document willingly and were of sound mind at the time of signing.
- In cases where a healthcare proxy, guardian, or power of attorney is authorized to complete the form on your behalf, ensure they sign in the designated area and fill in their relationship to you.
- Finally, submit the completed form as instructed. This may involve providing copies to your primary care physician, local hospital, or keeping it in a readily accessible place in your home.
Once the form is accurately filled out and submitted according to the given instructions, it becomes a legal directive for healthcare professionals to follow in the event of an emergency. It's recommended to review and, if necessary, update your DNR Order periodically or after any major health changes. This ensures that your end-of-life care preferences are always up-to-date.
Get Answers on Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR)?
A Do Not Resuscitate Order, commonly referred to as a DNR, is a medical directive written by a doctor which states that cardiopulmonary resuscitation (CPR) should not be performed in the event the patient's heart stops or if the patient stops breathing. This order is made at the patient's request or, if the patient is unable to make decisions, at the request of the patient's health proxy or a family member.
How does one obtain a DNR order?
To obtain a DNR order, a patient must discuss their wishes with their doctor. The doctor will then assess the patient's condition and overall health to ensure that a DNR order aligns with the patient's health care needs and desires. Once agreed upon, the doctor will fill out the DNR form, which must be signed by the patient or their legal representative. It's important to keep the original document easily accessible in case of an emergency.
Is a DNR order applicable in all healthcare settings?
No, a DNR order is primarily applicable in hospital settings. However, most states have protocols that extend the recognition of DNR orders to other settings such as nursing homes, assisted living facilities, and at home. It's essential to note that specific procedures and forms may vary by state to ensure a DNR is valid outside of a hospital. For example, some states require a separate form or identifier, such as a bracelet, to signify an out-of-hospital DNR.
Can a DNR order be revoked or changed?
Yes, a DNR order can be revoked or changed at any time by the patient if they are mentally competent to make healthcare decisions. To revoke a DNR, the patient should inform their doctor of their decision, and the doctor will then update the patient's medical records accordingly. If changing a DNR preference, a new order needs to be filled out and signed. When a DNR is revoked or altered, it's crucial to also update any copies that might be held by family members, healthcare proxies, or in personal files to reflect the changes.
Common mistakes
Filling out a Do Not Resuscitate (DNR) Order is a crucial step for individuals who wish to have their end-of-life medical wishes known. However, several common mistakes can undermine the effectiveness of these forms. Recognizing and avoiding these errors is essential for ensuring that the individual's preferences are honored.
One common mistake is neglecting to discuss the DNR order with family members and healthcare providers. This communication is vital to ensure that everyone involved understands the individual's wishes. When these conversations don't happen, it can lead to confusion and potential disputes among family members and medical personnel at critical moments.
Another error involves not having the DNR order signed by the required parties. Typically, this includes the individual for whom the DNR applies and their physician. Without these critical signatures, the document may not be considered valid, which could lead to unwanted medical interventions.
Some people mistakenly believe that a DNR order is included in a standard will or advanced directive without explicitly stating so. A DNR order is a separate document that needs specific mention and must be properly integrated with other estate planning documents to ensure wishes are clearly defined and legally recognized.
Failing to renew or update the DNR order as needed is another oversight. Changes in health condition, medical advancements, or personal preferences may necessitate modifications to the order. Regular reviews with healthcare providers ensure the DNR order reflects the current wishes and medical circumstances of the individual.
Incorrect filing of the DNR order can also pose a significant problem. If the document is not easily accessible, especially in an emergency, it may not be followed. Ensuring the DNR order is on file with one's physician, in addition to having copies in easily accessible places at home, can avoid this pitfall.
Many people also fail to carry a wallet card or wear some form of identification that alerts first responders to the presence of a DNR order. In emergencies outside the home, this can lead to unnecessary resuscitation efforts, contrary to the individual's wishes.
Choosing the wrong type of DNR order for one's specific situation can also lead to unwanted outcomes. Some states offer different forms for in-hospital and out-of-hospital situations. Not understanding the distinctions and choosing incorrectly can mean your wishes are not honored in the setting where you find yourself.
Lastly, assuming all states recognize a DNR order in the same way is a mistake. Legal requirements and recognition can vary significantly from one state to another. It’s important for individuals to ensure their DNR orders comply with the specific laws of their state or any state they may be traveling to.
Avoiding these mistakes requires careful preparation, discussion, and consultation with legal and medical professionals. Taking these steps helps ensure that a DNR order will be effective and that an individual's end-of-life wishes will be respected.
Documents used along the form
When planning for medical care in situations where one may not be able to make decisions personally, a Do Not Resuscitate (DNR) Order form is often emphasized. This critical document specifies the wish not to have cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. In conjunction with a DNR, there are several other important legal documents that can help ensure a person's healthcare preferences are respected and communicated to family members and healthcare providers.
- Advanced Directive: This legal document outlines an individual's preferences regarding medical treatments they want or wish to avoid, should they become unable to make decisions for themselves. It can include instructions on the use of life-sustaining measures.
- Health Care Proxy or Power of Attorney: This designates someone else, usually a trusted family member or friend, to make health care decisions if the individual is unable. This includes decisions beyond those detailed in an advanced directive.
- Living Will: Specific to end-of-life care, a living will details which medical interventions an individual wants or does not want if they're terminally ill or in a permanent vegetative state and cannot communicate their preferences.
- Physician Orders for Life-Sustaining Treatment (POLST): This medical order addresses other aspects of end-of-life treatment, such as intubation, antibiotic use, and feeding tubes, and is intended for seriously ill patients for whom a healthcare provider believes a natural death is imminent.
- Medical Orders for Scope of Treatment (MOST): Similar to a POLST, this is a doctor's order that delineates a patient's wishes regarding various life-sustaining treatments and interventions, tailored to those with serious illnesses.
- Organ and Tissue Donation Registration Form: This document records an individual's desire to donate organs and tissues after death. It is crucial for ensuring that these wishes are respected and can be acted upon promptly.
Each of these documents plays a vital role in healthcare planning, complementing a DNR by providing comprehensive guidance on a patient's preferences for treatment and intervention at the end of life. They ensure that healthcare providers and loved ones understand and respect the patient's wishes, facilitating peace of mind for all involved. It is advisable for individuals to discuss these forms with a healthcare provider and legal advisor to make informed decisions tailored to their personal beliefs and medical circumstances.
Similar forms
A Living Will shares similarities with a Do Not Resuscitate (DNR) Order in that both express an individual's medical treatment preferences in advance, particularly concerning end-of-life care. While a DNR specifically instructs healthcare providers not to perform CPR (cardiopulmonary resuscitation) if a person's breathing or heartbeat stops, a Living Will is broader, covering a range of life-sustaining treatments the individual wants or does not want if they are unable to communicate their wishes due to a severe health condition. Both documents serve as crucial tools in ensuring an individual's healthcare preferences are respected when they cannot speak for themselves.
Healthcare Power of Attorney (POA) forms also have a close correlation to DNR Orders. A Healthcare POA appoints someone else, typically a trusted family member or friend, to make health-related decisions on behalf of the individual if they become incapacitated. Like a DNR, which conveys specific instructions about not receiving CPR, a Healthcare POA can include directives about a variety of medical treatments and care preferences. However, its scope is broader, granting the appointed agent the authority to make healthcare decisions that might not be explicitly covered in a DNR or Living Will.
An Advance Healthcare Directive can be thought of as a combination of a Living Will and a Healthcare Power of Attorney. It delineates an individual's medical treatment preferences, much like a Living Will, and appoints a healthcare proxy or agent, similar to a Healthcare POA. This ensures that if individuals find themselves in situations where they cannot express their wishes, their predefined healthcare preferences are followed, and someone they trust is in place to oversee these choices being respected. An Advance Directive, therefore, encompasses the foresight of a DNR by allowing one to detail specific treatments like resuscitation that they wish to avoid.
Finally, a POLST (Physician Orders for Life-Sustaining Treatment) form is akin to a DNR but is more comprehensive in the range of medical interventions it addresses. It is a medical order that outlines a plan of care respecting the patient’s wishes concerning life-sustaining treatments, including intubation, mechanical ventilation, and artificial nutrition, in addition to CPR. POLST forms are intended for seriously ill or frail individuals for whom healthcare professionals believe CPR would be harmful, and they are recognized in various states. Both POLST forms and DNR orders ensure that a patient's preferences regarding emergency and other life-sustaining treatments are clearly communicated to healthcare providers.
Dos and Don'ts
When dealing with a Do Not Resuscitate (DNR) Order form, accuracy and clarity are paramount. These forms are critical in communicating a patient's wishes regarding life-saving treatments. Below are ten vital dos and don'ts to observe when completing a DNR form.
- Do ensure the person filling out the form fully understands the patient's wishes.
- Do have all necessary parties, including the patient (if capable) and healthcare providers, sign the form to validate its legality.
- Do verify that the form meets state-specific requirements, as laws can vary significantly from one jurisdiction to another.
- Do keep the DNR form in an easily accessible location for emergency responders.
- Do discuss the implications of a DNR order with a healthcare professional to ensure it is the best option for the patient's situation.
- Don't fill out the form without the consensus of the patient, if they are capable, or their legal healthcare proxy.
- Don't assume all healthcare facilities use the same form; always use the most current version specific to your state or facility.
- Don't leave blank sections or unanswered questions in the form, as this could lead to confusion or the document being considered invalid.
- Don't forget to update the form if the patient's health situation or wishes change.
- Don't fail to communicate with family members and loved ones about the existence and content of the DNR order to avoid surprises or conflicts during emergencies.
Misconceptions
When it comes to Do Not Resuscitate (DNR) Orders, there are several misconceptions that can cloud people's understanding and decision-making. Here's a list that clarifies some of these common misunderstandings:
Only the elderly can have a DNR order. People of any age can have a DNR order based on their health condition and preferences, not just those who are older.
A DNR order means no medical treatment will be provided. A DNR specifically refers to not performing CPR (cardiopulmonary resuscitation) if the heart stops or if breathing stops. Patients with a DNR order still receive other forms of medical care unless otherwise specified.
Doctors decide if someone gets a DNR order. While doctors can provide advice, the decision to have a DNR order is ultimately up to the patient or their legal healthcare proxy based on the patient’s wishes.
A DNR order cannot be changed once it's implemented. Patients or their healthcare proxies can change a DNR order at any time based on changes in the patient's health condition or preferences.
DNR orders are only for the hospital. DNR orders can also be applied in non-hospital settings, such as at home. It's important to make sure the DNR order is visible to emergency personnel in these settings.
Having a DNR order means giving up on life. Choosing a DNR order can be a decision to avoid unnecessary suffering and to die with dignity. It’s a personal choice based on individual values and medical conditions.
A DNR order is the same as an advance directive. A DNR is a specific medical order about CPR, whereas an advance directive is a broader document that can include various medical decisions, including a DNR preference.
If I’m healthy, I don’t need to think about a DNR order. It’s wise for people to consider all their healthcare options, including DNR orders, as part of broader advance care planning. This encourages discussions with family and healthcare providers about your values and wishes in case of future incapacity.
Key takeaways
Understanding and having a Do Not Resuscitate (DNR) order can be an important step for those wishing to have their healthcare preferences respected during critical moments. To ensure that your wishes are clearly communicated and honored, consider the following key takeaways:
- Clear Communication: A DNR order allows individuals to make their wishes known regarding CPR (cardiopulmonary resuscitation) in the event their heart stops or they stop breathing. This decision should be communicated clearly with family members and healthcare providers ahead of time.
- Physician's Role: For a DNR order to be valid, it must be signed by a physician. This signifies that the doctor has discussed the full implications of the DNR order with the individual (or their authorized healthcare agent) and agrees with their wishes.
- Legally Binding: Once signed, a DNR order is a legally binding document. Emergency personnel and healthcare providers are required to follow the instructions provided, given that the order is presented or is accessible during an emergency.
- Reassessing the Decision: Circumstances and perspectives can change over time. Individuals are encouraged to regularly review and discuss their DNR decisions with their doctor and amend them if their health status or preferences change.
- State-Specific Forms: It is important to note that DNR orders and regulations can vary from one state to another. Make sure to use the appropriate state-specific form and comply with its requirements.
- Accessibility: After completing the DNR form, it should be kept in an easily accessible location. Copies should be given to family members, healthcare proxies, or anyone who might be responsible for making healthcare decisions on the individual’s behalf.
- Emergency Situations: In emergencies, healthcare providers typically do everything possible to save a person’s life. Without a DNR order immediately available, emergency responders are required to proceed with all resuscitative efforts.
By keeping these considerations in mind, individuals can ensure that their healthcare preferences regarding resuscitation are understood and respected in critical situations. Planning ahead and having open discussions about DNR orders can provide peace of mind for everyone involved.
Other Templates:
Does California Have a Transfer on Death Deed - It empowers property owners to make definitive arrangements about who will receive their property, ensuring their legacy is honored.
Free Roommate Agreement - Brings clarity to the division of utilities and expenses, ensuring tenants know what they are responsible for outside of rent.
Free Deed of Trust Template - By clearly delineating the sequence of actions in case of default, it provides a predefined path for resolving loan repayment failures.